Will a Texas Hospital Abort a Baby if Mother Is a Suicide Risk
Miscarriages are extremely mutual, occurring in upwards to an estimated xxx% of all pregnancies. Nevertheless, pregnancy loss is oft poorly understood and conflated with induced abortions; for example, terms like "induced miscarriage" have been used to imply intent to end pregnancy, while "spontaneous abortion" is a medical term for a miscarriage. This cursory clarifies how pregnancy loss is singled-out from abortion, while highlighting the similarities in their management. Information technology also focuses on how abortion policies may touch on miscarriage care. At a fourth dimension when abortion restrictions effectually the country are increasing, laws may limit providers' power to manage pregnancy loss and that women experiencing pregnancy loss may be investigated to prove their miscarriages were unintentional. This brief examines how policies aimed at limiting abortion may have negative consequences on people experiencing pregnancy loss.
A Note on Terminology: a basic agreement of homo development is important in understanding pregnancy loss, its policy implications and its portrayal in the media. Pregnancies are dated using gestational age (GA), calculated by the time since the individual's last menstrual period (LMP) or past ultrasound if LMP is unknown. Fertilization, when a sperm fuses with an egg, occurs approximately ii weeks later menses, meaning GA predates fertilization past ~2 weeks. Therefore, from 0-2 weeks GA, the private is not even so meaning.
Around 4 weeks GA, the fertilized egg implants in the uterus. This roughly coincides with the commencement missed menstruation, and when a home pregnancy test would plow positive. Effectually 6 weeks GA, the developing heart is chosen a primitive heart tube due to its tubular shape, and develops detectable spontaneous cardiac activity. Appendix A outlines a brief timeline of cardiac evolution.
From 5-10 weeks GA, the term "embryo" describes the developing pregnancy, while "fetus" is used from eleven weeks GA onwards. Additional terms are defined in the Glossary.
Sources: U.S National Library of Medicine. Fetal Evolution. Updated 10/02/2019; ACOG. How Your Fetus Grows During Pregnancy. April 2018; Rice University. Development of the Eye. Anatomy and Physiology.
What is pregnancy loss?
How pregnancy loss is categorized largely depends on when in the pregnancy it occurred. The U.South. medical customs most often defines miscarriage (too called spontaneous abortion) equally the spontaneous loss of a nonviable, intrauterine pregnancy before 20 weeks gestational age (GA), while stillbirth (also chosen fetal death and intrauterine fetal demise) describes this event at ≥ xx weeks GA. A belatedly stillbirth or late intrauterine fetal demise occurs after 28 weeks. Pregnancy loss serves equally an umbrella term for all gestational ages (see Glossary for definitions of non-feasible and intrauterine). Consensus effectually these terms does not fully exist; for instance, other countries use different gestational ages to distinguish miscarriage from stillbirth, while many journalists use miscarriage to draw pregnancy loss at any stage of pregnancy. The terms miscarriage and stillbirth take been institute to be preferred by people experiencing these events, therefore will be used in this brief equally opposed to culling terms (Appendix B).
Common symptoms of pregnancy loss include vaginal haemorrhage and cramping, which may prompt presentation to a healthcare facility. Alternatively, some miscarriages and stillbirths accept no symptoms and are discovered during routine prenatal care (for example, when cardiac action cannot be found).
How are miscarriages dissimilar from abortions?
Medical providers ofttimes refer to miscarriages as spontaneous abortions, or by its subcategories including missed, incomplete and inevitable abortions (see Glossary). These terms are distinct from a voluntary termination of a pregnancy, unremarkably referred to as an abortion, or equally an "induced or therapeutic" ballgame in medical terms. Despite this, lawmakers have used "induced miscarriage" or "procuring a miscarriage" to draw intentional attempts to terminate a pregnancy, exemplifying how miscarriage and abortion are easily conflated. To clarify, miscarriages and stillbirths refer to the spontaneous death of an embryo or fetus, but not to the elective termination of pregnancy.
How common is pregnancy loss?
Miscarriages are extremely common, despite public perception that pregnancy loss is rare. Approximately ten-xx% of pregnancies confirmed by testing result in a miscarriage by xiii weeks GA, only estimates are as high as 31% to 50% when including individuals who miscarry before knowing they are pregnant.i The vast majority of all pregnancy losses occur before thirteen weeks (~80%). Pregnancy loss afterward in pregnancy is less common; approximately one% of all pregnancies finish in miscarriage between xiii-twenty weeks and less than 1% of pregnancies end in stillbirth after 20 weeks. Miscarriages are increasingly common as maternal age increases (Figure one). A pregnant portion of women volition experience a pregnancy loss in their lifetime, but most will go on to accept healthy pregnancies thereafter.
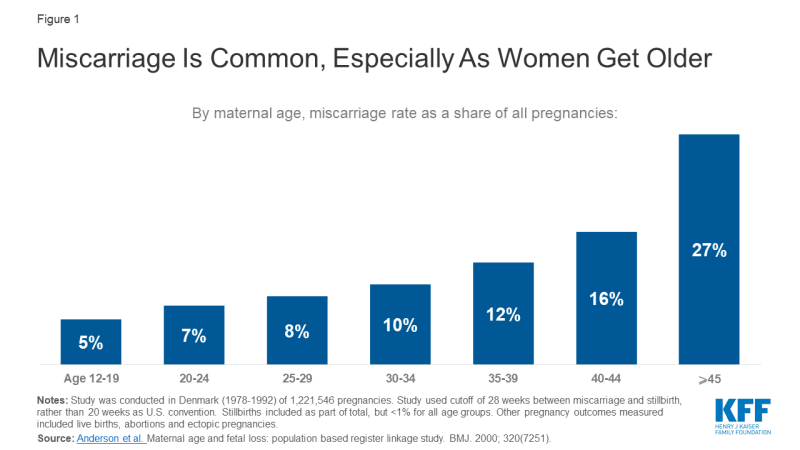
Figure one: Miscarriage Is Common, Particularly Every bit Women Become Older
What causes pregnancy loss?
More often than not, the cause of a pregnancy loss is unknown even later thorough evaluation. Of those with a suspected cause, the bulk of miscarriages are attributed to genetic abnormalities (50-70%), and less commonly uterine cavity distortion (fibroids, adhesions, etc.), autoimmune and clotting disorders. Similarly, nearly stillbirths are caused by genetic abnormalities, problems with the placenta, fetal growth restriction or infection.two Risk factors for pregnancy loss include maternal age <20 or >35 years old, non-Hispanic Blackness race, diabetes, obesity, tobacco use (both maternal and paternal exposure) and certain illicit drug use. However, take a chance factors practise not cause pregnancy loss, thus a significant person with one or more of these risk factors should non be faulted for their pregnancy loss. Providing psychological support for those experiencing these events is of import, as many people feel guilty, solitary or ashamed.
How do abortion restrictions impact how pregnancy loss is managed?
Recent legislation restricting abortion and increasing laws and regulations designed to provide "fetal protection" can impact patients experiencing pregnancy loss. Below nosotros outline how restrictions aimed at ballgame may have consequences for pregnancy loss care, focusing on training, handling and legal implications.
Grooming
Depending on the stage in pregnancy, the patient preferences, and the clinical scenario, patients experiencing pregnancy loss tin can be treated with (1) expectant management, (2) medications, like misoprostol with or without mifepristone, or (3) a surgical procedure, either uterine aspiration or dilation and evacuation (D&Due east) (Tabular array one).
| Table one: How Pregnancy Loss Can Be Managed at Various Stages in Pregnancy | |||
| Method | Clarification | Example situations | |
| Earlier in pregnancy Later in pregnancy | Expectant Direction | Wait for nonviable pregnancy tissue to laissez passer on its own from the uterus. Safe up to ~8 weeks GA. | For individuals who want to non-invasively manage their miscarriage at home and are medically stable, without contraindications. About 80% of miscarriages will complete on their own in 8 weeks. |
| Medical Management (for miscarriage) | Facilitate passage of nonviable pregnancy tissue from the uterus, typically with misoprostol +/- mifepristone. | In early pregnancy, allows shorter time course than expectant management in patients without complications. Treatment with misoprostol results in complete passage of the non-viable pregnancy within ii days in about cases. | |
| Uterine aspiration/ Suction curettage | Dilation of cervix and aspiration of nonviable pregnancy tissue from uterus. Tin can be used up to fourteen-16 weeks gestation. | For individuals who are medically unstable, or have incomplete miscarriage after expectant or medical management or want prompt resolution of miscarriage. Typically an office process. | |
| Dilation and evacuation (D&East) | Dilation of neck and evacuation of stillborn with suction and/or forceps, typically used from fourteen weeks upwards until 28 weeks GA. | Ensures prompt passage of stillborn, does not require laboring, will typically be performed in an operating room with sedation. | |
| Labor induction (for stillbirth) | Induce onset of labor, typically with misoprostol +/- mifepristone. Patient will vaginally deliver stillborn. | For individuals with a stillbirth, who prefer to deliver stillborn (opportunity to view or concur). Performed in a hospital. | |
| NOTES: Example situations are non an exhaustive listing of indications for each management blazon. Hurting control and need for Rhogam should exist addressed for all patients, and grief counseling if needed. Many of the direction methods can likewise exist employed for induced abortions. SOURCES: ACOG practice bulletins on Early Pregnancy Loss and Management of Stillbirth. National Academies of Sciences, Engineering and Medicine. The Condom and Quality of Abortion Care in the U.S. 2018. Improving Educational activity in Reproductive Health. Early Pregnancy Loss Management. | |||
Most all of the methods used to manage miscarriages and stillbirths are identical to those used in therapeutic abortions. Therefore, the clinical training necessary to safely manage a patient experiencing a pregnancy loss is very similar to that needed to perform abortions. As such, medical residents at religiously affiliated hospitals or in states with restrictive abortion laws may struggle to obtain the necessary training and caseload to become skilful in these skills. Although miscarriage is mutual and information technology may seem as if physicians would easily obtain this training through managing pregnancy loss alone, research on this topic suggests otherwise; a report comparing U.South. OBGYN residency programs found that residents at programs with routine ballgame preparation were significantly more likely to receive grooming in D&Es (a direction option for pregnancy loss) as compared to those with optional or no ballgame preparation. Another study constitute physicians with prior ballgame training almost three times more likely to provide in-office uterine evacuations to patients experiencing pregnancy loss as compared to physicans without prior abortion training; lack of training was cited as a barrier to providing this service in cases of pregnancy loss by 16% of physicians without abortion training and just ii% of physicans with abortion preparation. When miscarriages nowadays in emergency settings with significant bleeding or infection, it is imperative the clinician has the skills to promptly and safely treat that individual. Little to no training in abortion care may negatively touch providers' ability to safely manage pregnancy loss.
Treatment
Limiting Medical Treatment Bachelor
While miscarriages tin can be managed with misoprostol alone, the combination of misoprostol and mifepristone is more constructive. In fact, the American College of Obstetricians and Gynecologists (ACOG) recommends combination therapy, but mifepristone's availability is limited due to its use in medication abortions. Mifepristone is subject to Risk Evaluation and Mitigation Strategy (REMS) restrictions,three requiring it exist dispensed only by certified providers in sure clinics and hospitals, rather than from a retail chemist's. This can be problematic for many emergency rooms, master care or prenatal clinics where patients may be diagnosed with miscarriages, simply cannot be adequately treated because their healthcare setting does not stock mifepristone or lacks certified providers. For comparing, all doctors in Canada can prescribe mifepristone and it can be picked up in pharmacies. The REMS on Mifepristone impacts not just abortion care, just likewise limits miscarriage treatment equally well.
Some medications are used in pregnancy loss, abortions and pregnancy. What practise these drugs practice?
Misoprostol: Softens/relaxes the cervix and causes uterine contractions. Multiple uses in obstetrics and gynecology for labor induction, pregnancy loss, medication ballgame, postpartum hemorrhage and before surgical procedures. Also used to preclude gastric ulcers.
Mifepristone (Mifeprex): Blocks the activeness of progesterone, causing the uterine lining to destabilize and stops progression of existing pregnancy. Used in medication abortions, miscarriages and less frequently, for emergency contraception, endometriosis, fibroids and to induce labor.
Oxytocin (Pitocin): Causes uterine contractions. Used to induce labor, treat postpartum hemorrhage and pregnancy loss, and sometimes to help uterus contract later abortions.
Limiting Surgical Handling Available
Many states prohibit certain surgical methods for abortion, which may limit services for pregnancy loss. Based on the Fractional-Nativity Ballgame Ban Deed of 2003 and Gonzalez 5. Carhart (2007), xx states have enacted bans on so-called "partial nascency abortion," except when necessary to salve the life of the female parent. "Partial nascence abortion" is not a medical term, but is used by policymakers to refer to the rarely used dilation and extraction (D&X) procedure (see Glossary). D&X can be used in abortion simply besides in stillbirth management if the intact stillborn is desired past the family unit for personal reasons (religious, burying anniversary, etc.) or medical reasons to assess cause of death. These policies have also been interpreted more broadly to prohibit D&E procedures, used ordinarily in pregnancy loss and abortion direction; D&E bans are enacted in Mississippi and Westward Virginia, and temporarily enjoined in 6 other states (AR, KS, KY, LA, OH, OK) (Effigy 2).
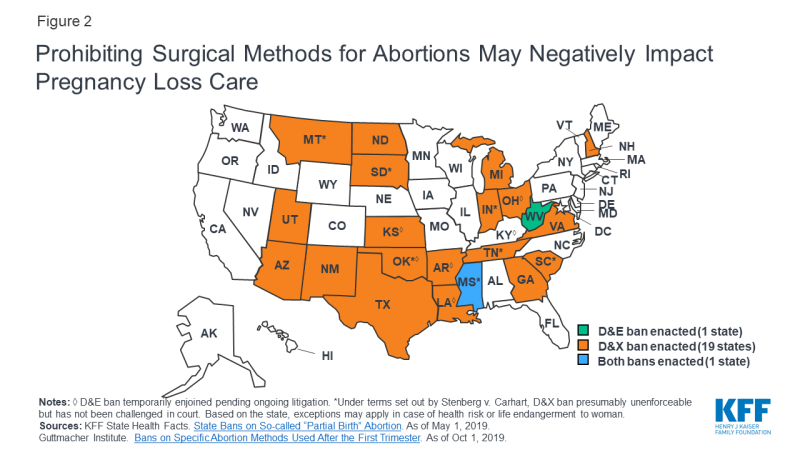
Figure 2: Prohibiting Surgical Methods for Abortions May Negatively Bear upon Pregnancy Loss Care
D&X and D&Eastward bans include language prohibiting these procedures on a "living unborn child" or
"living fetus" [non-medical terms], therefore practice not explicitly prohibit these procedures for use in stillbirths. Under less common circumstances, however, fetal cardiac activity may be nowadays during cases of miscarriage (Glossary), preventing the above procedures from being used where bans apply. For example, a patient with a pre-viable fetus at twenty weeks gestation may have a completely dilated cervix (meaning the pregnancy loss is inevitable) and be bleeding significantly, only denied surgical management until the fetus no longer has a heartbeat or until the situation is life threatening. A study of Catholic-owned hospitals documented several cases of patients who were actively miscarrying and denied uterine evacuation while cardiac activity was nevertheless detectable, leading to delays in care and transfers to outside hospitals. It is therefore possible that surgical bans on ballgame may limit medical determination making in nuanced cases of pregnancy loss.
Bans on D&Es and D&Xs for abortion may also cause providers to shy away from their use even for pregnancy loss management; providers may exist fearful to provide these services due to perceived legal ramifications and may become less practiced and adept in D&Eastward procedures over time, fifty-fifty when performed for pregnancy loss. For stillbirths, the alternative to surgical direction is induction of labor with medications; this has been shown to be less prophylactic for the mother than D&Es and ofttimes requires a multi-day hospitalization.
Confidentiality and Privacy Concerns: Altering the Patient-Provider Relationship
People experiencing pregnancy loss may be deterred from seeking medical care, especially in places hostile to abortion. For example, individuals may be investigated to ensure there was no intent to stop the pregnancy. Every bit of 2019, If/When/How Legal Team4 found vi states with laws retained from before Roe five. Wade that straight criminalize self-managed abortions (AZ, DE, ID, NV, OK, SC),5 and examples of their enforcement after 1973. Meanwhile 10 states have laws criminalizing fetal harm without explicit exemptions for significant people (Effigy 3); these take been applied in cases of attempted maternal suicide and self-managed abortion, amidst other examples. These same laws are presumably enforceable until repealed or enjoined; in at least twenty states since Roe v. Wade, criminal investigations or arrests have been made for alleged self-managed abortion (Figure 4), all the same it is unclear how many of these women were ultimately charged, and how many were establish to be cocky-managed abortions verses pregnancy losses.
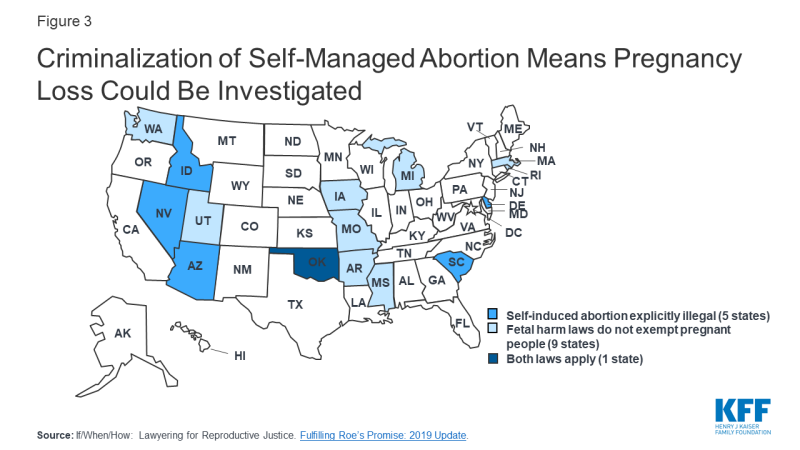
Figure 3: Criminalization of Self-Managed Abortion Means Pregnancy Loss Could Be Investigated

Figure 4: Alleged Self-Managed Abortion Prompts Arrests and Criminal Investigations in Many States
These laws can be problematic for patients experiencing pregnancy loss, as they could prompt healthcare providers to report patients to police force enforcement after pregnancy loss. In that location have been several cases where hospital workers have called the constabulary on patients after suspecting intent to cease their pregnancy, calling patient-provider confidentiality into question. This could brand pregnant people who always expressed ambivalence about their pregnancy vulnerable to investigation; a recent written report showed ~xxx% of women entering prenatal care considered an ballgame for their electric current pregnancy.
Several states accept proposed requiring reporting of miscarriages. Kansas proposed a requirement for miscarriages and stillbirths to be reported to the state, while Virginia attempted to mandate reporting of pregnancy loss to law enforcement, including the proper noun of the mother and the location of the pregnancy remains. Mandated reporting could impact patient-provider confidentiality, and may event in some some women delaying seeking care until they are in emergency situations. Many medical groups, including ACOG, the American Medical Association and Physicians for Reproductive Health, oppose criminalization of self-managed abortion and oppose mandated reporting by clinicians if a self-managed abortion is suspected.
How tin abortion restrictions event in the criminalization of pregnancy loss?
We highlight beneath how legislation surrounding personhood, fetal homicide and substance employ in pregnancy has been used to criminalize women who experience pregnancy loss and the clinicians that manage their care.
What is "Fetal Protection" legislation?
"Personhood" laws seek to grant total personhood, and thus full protection under the constabulary, to the earliest stages of homo development, including fertilized eggs. The push for "personhood" laws has increased in contempo years; in May 2019, Alabama passed into police the Human Life Protection Act, defining a person as including an "unborn child in utero at whatever stage of development." Georgia similarly included personhood language in the LIFE Act, which would ban abortion after the detection of cardiac action, but neither the Alabama and Georgia laws are currently in effect while being challenged in court. Colorado, Mississippi, Oklahoma, North Dakota and Kansas have too introduced legislation to grant personhood rights as early equally fertilization, however were not enacted.
Other types of "fetal protection" legislation be. As of May 2018, 38 states had fetal homicide laws distinguishing the expiry of the developing pregnancy from the death of the pregnant person; in 29 states, these laws apply to all stages of pregnancy. While these laws are typically applied against people who commit tearing crimes towards pregnant women, they tin can also exist used against pregnant people themselves in states without explicit exemptions. Co-ordinate to an analysis of state fetal homicide laws, as of 2014 at least 7 states did not include maternal exemptions for electric current pregnancies in their fetal harm laws.
I effect of "fetal protection" legislation is that by granting full rights to a fertilized egg, embryo or fetus, or by failing to provide sufficient exemptions to meaning women in fetal harm laws, the rights and protections of the pregnant individual may inevitably decrease. Considering the pregnant person and their developing pregnancy can be regarded past the constabulary as two separate entities, if a person experiences a pregnancy loss and they are thought to be at error in whatever way, they could be charged with a crime using fetal protection legislation. This exposes significant people to possible investigations equally to how their actions (substance use, medication use, exercise, diet, lifestyle, etc.) or inactions (missing prenatal intendance appointments, not taking prenatal supplements, etc.) during pregnancy may take led to their pregnancy loss. It remains uncertain whether fetal protection legislation may exist used in the future to protect or criminalize pregnant individuals.
How has Pregnancy Loss been criminalized using such legislation?
At that place is a long history in the U.S. in which women have been criminalized for their ain miscarriages or stillbirths. The National Advocates for Significant Women identified more than than 400 criminal and ceremonious cases from 1973-2005 in which a woman'due south pregnancy was a necessary factor in the charge against her; sixty-8 of these cases involved a miscarriage, stillbirth or baby death attributed to the woman's deportment or inactions during pregnancy. While many of these cases did not mention any intent to end the pregnancy, they nonetheless resulted in charges including feticide, manslaughter, reckless homicide, child abuse and get-go-degree murder. The women involved were overwhelmingly low-income and women of color, highlighting racial and economic disparities in the legal system and healthcare. Below, we outline how individuals accept been charged with crimes relating to their pregnancy losses subsequently experiencing trauma, failing medical advice and using both legal and illicit drugs in pregnancy.
Experiencing Physical Trauma in Pregnancy
Employing fetal protection legislation, multiple women who experienced physical trauma during pregnancy take been charged with manslaughter after subsequent pregnancy loss or neonatal death. Various states have charged women with crimes related to their pregnancy loss in the setting of being shot in the abdomen, unintentionally falling down stairs, attempting suicide and existence in car accidents, equally it was thought they put their fetuses in damage's way. While several of these charges were eventually dropped, some of these women take served jail time or prison house sentences. This occurred recently in Alabama for a woman who experienced a stillbirth at 5 months after beingness shot in the abdomen; she was initially charged with manslaughter of the fetus, every bit she was thought to have provoked the fight that resulted in her being shot.6
Declining Medical Advice in Pregnancy
Several women who experienced stillbirths have been charged with murder under the rationale that if they had sought or adhered with medical care before they would have delivered healthy babies. In 1 such case, a women who opted for a midwife-assisted home delivery delivered a stillborn and was charged with reckless homicide for not presenting to the hospital for a cesarean delivery. Another women pregnant with twins (i lived, one delivered stillborn) was charged with murder for declining a recommended cesarean section. These cases highlight how being meaning may be used in medical decision making and the constabulary to limit maternal rights and autonomy. Even if court ordered, ACOG opposes forced medical interventions on significant women, as they believe coercion exploits power differentials, and violates patients' rights and bodily integrity, specially in the case of surgery.
Substance Utilise in Pregnancy
The most common reason women are blamed for pregnancy loss is due to substance use. According to an investigation by ProPubilca, 45 states prosecuted women for drug utilize during pregnancy from 1973-2015, regardless of if the pregnancy was harmed or not. In Minnesota, South Dakota and Wisconsin, women who use drugs can be involuntarily detained in a treatment program during pregnancy, while 23 states and D.C. consider substance use in pregnancy to be child abuse (Figure five); every bit almost all medical professionals are mandated reporters of kid corruption, this has significant implications on confidentiality when pregnant individuals seek medical care.
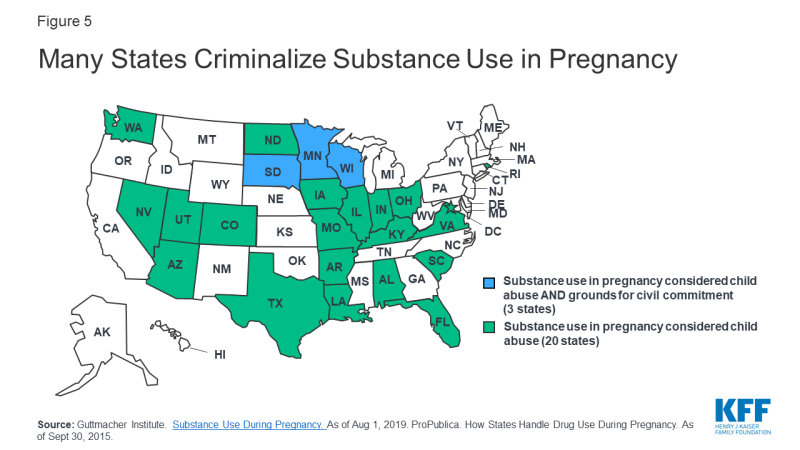
Figure 5: Many States Criminalize Substance Utilize in Pregnancy
Child abuse laws in South Carolina are particularly vague when it comes to pregnancy; in Whitner v. Land, kid corruption was adamant to include "maternal acts endangering or likely to endanger the life, condolement or health of a feasible fetus". Which "maternal acts" constitute child abuse has been left open up to interpretation, but have oftentimes been applied in the context of illegal drug use.
Alabama too penalizes meaning people who use drugs. Nether Alabama's Chemical Endangerment Law, drug utilize during pregnancy constitutes a Grade A felony in the upshot of a pregnancy loss, with a 10-99 year prison house sentence. They define knowingly exposing a child (including a fertilized egg, embryo or fetus) to a "controlled substance" or "chemical substance" as a crime, and as of 2015, 479 pregnant women were charged under this law due to in utero exposure to marijuana (24%), cocaine (22%), methamphetamines (18%) and opiates (14%). Other controlled substances include benzodiazepines (Xanax, Valium, Ativan) and many sleeping aids.
What almost legal substances? Some laws criminalizing apply of controlled substances in pregnancy do not distinguish betwixt prescribed medications and those obtained illicitly. This makes women prescribed opioids for chronic pain or medication-assisted handling (MAT) for opioid use disorder specially vulnerable. For example, a woman in Alabama faced 20 years in prison house and lost custody of her child after taking prescribed methadone during pregnancy.7 Meanwhile, a woman in Louisiana miscarried after receiving the contraceptive Depo-Provera from her doctor while unknowingly pregnant; she served over a year in jail for 2nd degree murder before charges were dropped. In 2016, Alabama signed into police force an exemption for women legally prescribed drugs from their chemical endangerment police. Despite this, greyness area still remains as to how the employ of legal, but not prescribed substances– similar cigarettes, alcohol, herbal remedies and supplements—could be criminalized during pregnancy.
What does substance employ inquiry say? While multiple court cases have concluded substance utilise caused the woman's pregnancy loss, the medical reality of these cases is typically less straightforward. Several confounders pose barriers to studying the touch of substance use on pregnancy loss. Poor nutrition, medical comorbidities and lack of prenatal care can all influence a healthy pregnancy, and are prevalent among people with substance use disorders. Effects of substance use in pregnancy likewise vary based on when in pregnancy the drug was taken, how often and at what dose. While decades of enquiry on substance employ and pregnancy take yielded mixed results, review of the literature suggests active cigarette smoking and methamphetamine use confer higher risks of pregnancy loss than in non-users. The relationship between pregnancy loss and alcohol8, marijuana, cocaine9, opiates and caffeine remains less clear. Information technology should be emphasized that substance utilize is considered a adventure factor for pregnancy loss, only has rarely been identified as the direct cause of pregnancy loss.
What does the medical community say? ACOG has urged state legislators to retract laws punishing women for substance use in pregnancy, stating that punitive legal efforts are inappropriate and ineffective to address substance use disorders. Similarly, the American Medical Clan (AMA), the American Nurses Association (ANA), the American Public Wellness Clan (APHA), the American Society of Habit Medicine (ASAM) and multiple other medical organizations oppose the criminalization of substance use disorder in pregnancy, as these policies deter women from prenatal intendance, confiding in medical providers and seeking substance apply disorder treatment.
Conclusions
Pregnancy loss is extremely common, and is sometimes conflated with abortion. Growing efforts to restrict abortion may create a medical and legal surround in which some pregnant people are discouraged from seeking medical care and are vulnerable criminalization if they feel pregnancy loss.
The authors would similar to acknowledge Jennifer Karlin, Dr., PhD (University of California, San Francisco) for her review of an before draft of this brief.
Will a Texas Hospital Abort a Baby if Mother Is a Suicide Risk
Source: https://www.kff.org/womens-health-policy/issue-brief/understanding-pregnancy-loss-in-the-context-of-abortion-restrictions-and-fetal-harm-laws/
0 Response to "Will a Texas Hospital Abort a Baby if Mother Is a Suicide Risk"
Post a Comment